By Dr. Jessie Wai Leng Phoon, MRCOG
Medical Director, GenPrime Fertility Singapore
Last reviewed: January 2026
Pregnancy is usually a time when care is focused on the baby. So when an unexpected cancer diagnosis appears during or after delivery, it can be deeply unsettling—especially when it involves the uterus.
One such condition is uterine leiomyosarcoma, a very rare and aggressive cancer that can sometimes be discovered unexpectedly during pregnancy or childbirth.
This article explains what uterine leiomyosarcoma is, why it can be difficult to detect during pregnancy, and what patients should understand if they have fibroids that change during pregnancy. It is based on a published case report from Singapore and broader clinical experience.
Leiomyosarcoma in pregnancy
What is uterine leiomyosarcoma?
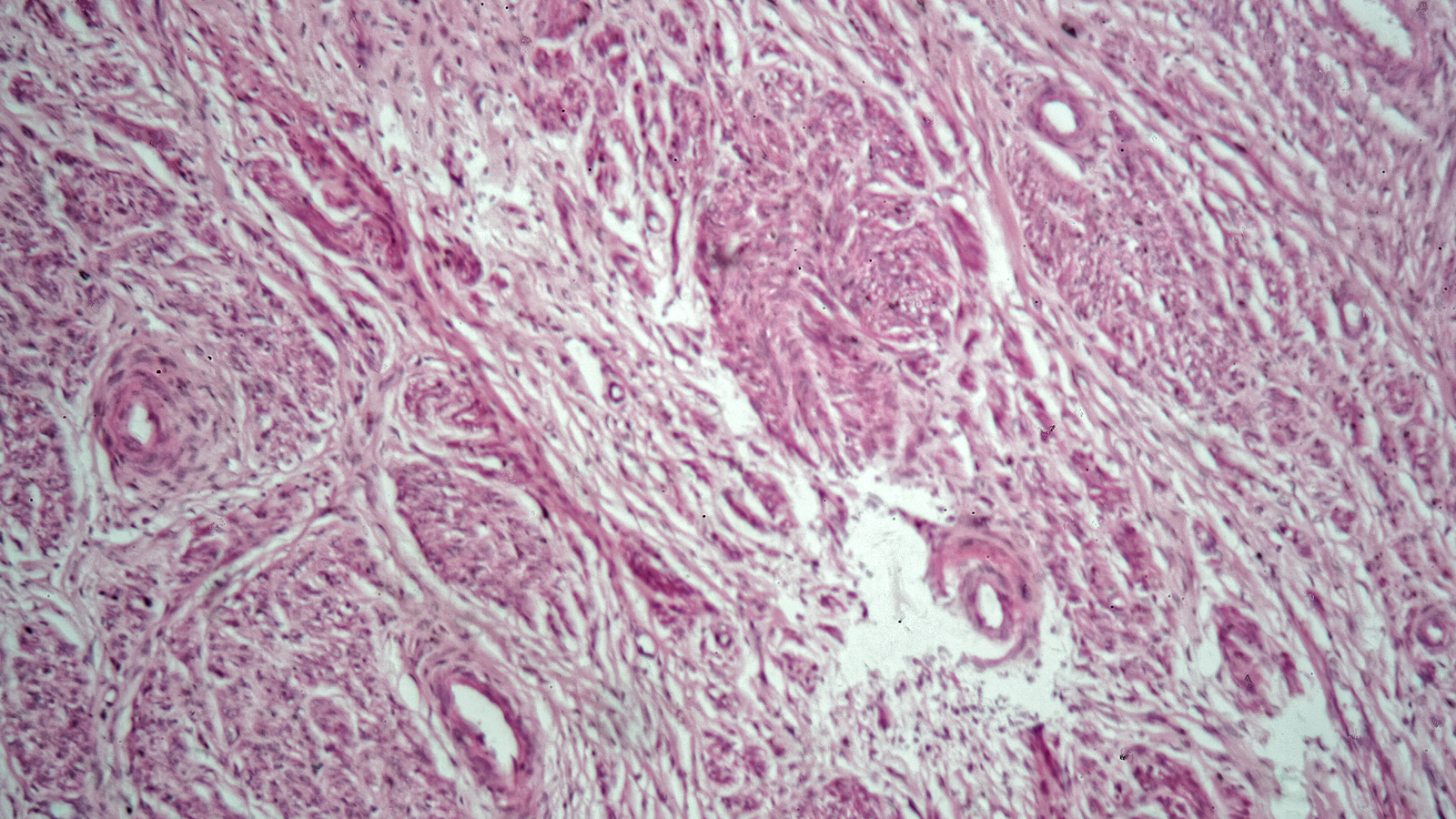
Uterine leiomyosarcoma (LMS) is a rare cancer of the smooth muscle of the uterus. It accounts for only a small percentage of uterine cancers and is very different from common uterine fibroids (leiomyomas), which are benign.
Key points to know:
- LMS is uncommon, especially in women of childbearing age
- It tends to behave aggressively
- It cannot be reliably diagnosed without surgical removal and histological examination
Because of this, LMS is often diagnosed only after surgery, when tissue is examined under a microscope.
How rare is leiomyosarcoma in pregnancy?
Leiomyosarcoma occurring during pregnancy is extremely rare. Fewer than a dozen cases have been reported in medical literature worldwide.
In most documented cases:
- The cancer was not suspected during pregnancy
- The uterine mass was thought to be a fibroid
- The diagnosis was made incidentally, often after caesarean section or myomectomy
This rarity is important context—most fibroids in pregnancy are benign.
Why leiomyosarcoma is difficult to detect during pregnancy?
Pregnancy itself causes hormonal changes that can make fibroids:
- Enlarge
- Change in appearance on ultrasound
- Become more symptomatic
This overlap makes it difficult to distinguish benign fibroids from rare malignancies like LMS.
Even advanced imaging:
- Ultrasound may show atypical features, but these are not specific
- MRI can raise suspicion but cannot confirm the diagnosis
At present, there is no imaging test that can reliably rule out leiomyosarcoma before surgery.
What happened in the reported case?
In the published case:
- A woman with a known uterine fibroid became pregnant and was monitored throughout pregnancy
- The fibroid increased in size but showed no clear signs of malignancy
- During a planned caesarean section, the fibroid was easily accessible and removed
- Histology unexpectedly revealed high-grade uterine leiomyosarcoma
Following the diagnosis, the patient underwent:
- Completion surgery (removal of the uterus and ovaries)
- Close follow-up with imaging rather than chemotherapy, after careful counselling
At follow-up, there was no evidence of recurrence.
Should fibroids be removed during caesarean section?
Myomectomy (fibroid removal) during caesarean section is not routinely performed, mainly because of the risk of heavy bleeding.
However, in selected situations, removal may be considered:
- When the fibroid obstructs delivery
- When it is easily accessible
- When the uterus is well contracted
- When malignancy is a concern (though rare)
This decision must balance:
- Surgical safety
- Bleeding risk
- The patient’s future fertility wishes
- The very low—but real—risk of occult malignancy
There is no one-size-fits-all answer. Experience of the surgical team and patient counselling are critical.
What does this mean for women with fibroids in pregnancy?
For most women, fibroids in pregnancy are benign and manageable. However, this case highlights a few important considerations:
- Rapid growth of a fibroid in pregnancy is usually benign, but should be monitored
- Regular follow-up imaging is important
- Patients should be counselled that, very rarely, a fibroid may not be benign
- Decisions around surgery should involve shared decision-making
Importantly, the presence of fibroids alone should not cause alarm—leiomyosarcoma remains exceedingly rare.
Treatment of uterine leiomyosarcoma
The primary treatment for uterine leiomyosarcoma is surgery, typically involving:
- Removal of the uterus
- Removal of the ovaries in most cases
The role of additional treatments such as chemotherapy is less clear and depends on:
- Stage of the disease
- Tumour grade
- Patient preferences
Because evidence is limited and outcomes vary, management is usually discussed in a multidisciplinary tumour board setting.
Questions to ask your doctor
If you have fibroids during pregnancy or have been told about unexpected findings, you may want to ask:
- How often should my fibroid be monitored during pregnancy?
- Are there features that would raise concern for something other than a benign fibroid?
- Would removal during caesarean section ever be considered in my case?
- What are the risks of surgery versus leaving the fibroid in place?
- How would future fertility be affected by different management options?
A simple next step
If you have fibroids and are pregnant—or planning a pregnancy—the most important step is ongoing, individualised care.
Regular monitoring, clear communication, and shared decision-making with your obstetrician help ensure that rare conditions are recognised early, while avoiding unnecessary intervention for the vast majority of benign cases.
About the Author
Dr. Jessie Wai Leng Phoon, MRCOGDr Jessie Phoon is a leader in fertility innovation and integrated women’s health, blending advanced clinical training with a personal approach to care. A graduate of the University of Auckland, she is an MOH-accredited IVF specialist with expertise across assisted reproduction and minimally invasive surgery. She previously served as Director of KKIVF Centre and the National Sperm Bank, and co-founded Singapore’s pioneering OncoFertility Clinic.